Vital elderly people in the third phase of life are often expected to remain socially active and care for the ‘oldest old’. But what if older people live in vulnerable situations, face insecurity, and have no access to resources or social networks? How can policymakers and researchers reach this vulnerable group and involve them in meaningful participation?
Calls from researchers and policymakers to participate in research are often responded to by older people who are better educated and can tap into various resources in their environment. In contrast, research into meaningful participation of older people in vulnerable living situations is scarce. Policymakers and researchers quickly speak of ‘hard to reach groups’. But you may wonder whether it is not the case that one’s own methodology, social position and the institutions of which researchers are a part create a distance and an us-versus-them feeling that hinders contact.
Photographing your neighborhood
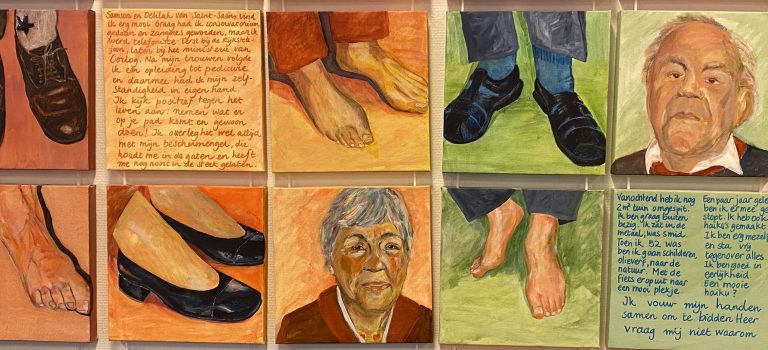
To find out what older people in vulnerable situations experience as meaningful participation, a research team from the Social and Cultural Planning Office (SCP) and Leyden Academy on Vitality and Ageing executed a participatory action research in two metropolitan neighborhoods: Amsterdam East and Laak in The Hague. The researchers formed a team in each neighborhood with older co-researchers, who examined their own lives and those of their fellow residents with a view to improving their living situation. In this photo-voice project, people photographed their neighborhood and their own lives under the guidance of artist Janine Schrijver. This provided clear images about the living environment of the participants.
Positive energy
To conclude this project, the older co-researchers discussed their photo stories with policy makers and researchers. It became clear that the participants found the energy to make their voices heard in their joint photo story project. “Sometimes it seems as if the relationship between government and citizens has run out of steam. This project shows that new positive energy can be created,” says Crétien van Campen, researcher at SCP and co-initiator. Co-initiator and director of Leyden Academy prof. dr. Tineke Abma, also emphasized the enthusiasm that this project has generated: “It is incredibly beautiful to see that it not only makes it clear where pain points are, but that this process also leads to connection. For example, an initiative in Amsterdam, which ensures that people who are isolated – especially women with a migration background – actively develop and maintain friendships again.”
Director of the SCP, Karen van Oudenhoven, even spoke about the bridge that this project has created between the language of citizens and the language of policy. “As researchers and policymakers, we are used to coming up with questionnaires and then processing the answers. But there is a large group that does not like it or even distances itself from it. How do you ensure that this group is heard and that their experience and opinions are included in decision-making? This project has proven that this is possible!”
Participatory research
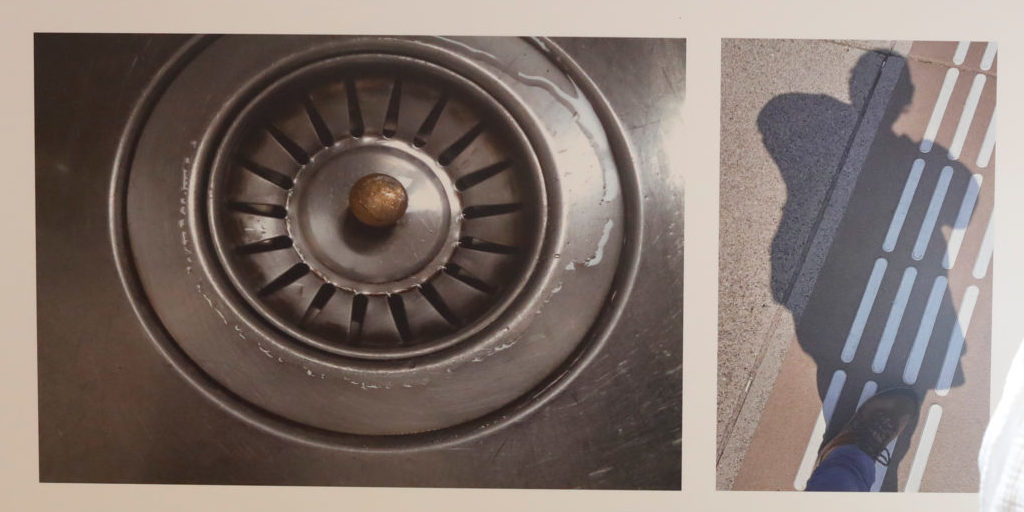
The photos in combination with a short text made it clear what people really encounter and what their wishes and needs are. For example, 63-years-old Lydia, she photographed a drain and a shadow of herself: “This is how I am treated by the government and that is how I often feel. I try to open people’s eyes about the informal care profession with my photos and story. Because that’s what it is, a profession. But without training and without being paid. People think too easily about informal care. It’s swim or drown.”
This innovative way of participatory research also appeals greatly to Wim Burggraaff, government policy advisor: “Instead of saying that they are difficult to reach, we should choose other paths. Normally I have a research report of many pages that I try to capture in one image where we move from ‘saying and thinking’ to ‘feeling and doing’. I therefore invite all researchers to collect many more stories in this way. Only then will we hear the voices of people we normally don’t hear.”
Key factors
The photo-voice project showed several key factors for successfully reaching and involving older people in vulnerable situations:
- The fact that the researchers knew the neighborhood, culture and language ensured that doors that were closed to anonymous research remained, now opened. Taking time for ‘normal’ conversations was crucial for building trust.
- By first creating space for conversation and attuning to the living environment of the residents, the elderly felt heard and seen.
- Empathy and letting go of your own working methods.
Reaching older people in vulnerable situations therefore requires a different approach by policymakers and researchers. Instead of labeling the elderly as ‘difficult to reach’, researchers and policy makers could take a more critical look at their own habits and actions that make contact difficult. For example, by choosing the photo-voice approach, elderly people in vulnerable situations can be given the space to make their voices heard and work together to improve their living conditions. In this way, the gap between institutions and vulnerable elderly people can be bridged.